Skin & Pressure Sores – Care, Treatment & Prevention after Spinal Cord Injury
Skin sores are the most common and devastating medical complication of spinal cord injury. Also called pressure sores, decubiti, decubitus ulcers, or bedsores, skin sores are more apt to occur after spinal cord iinjuries due to lack of movement and sensation and to changes in circulation.
The social impact of skin problems far outweighs almost all other problems you may encounter. A skin sore can mean several weeks of hospitalization or bed rest in order for the sore to heal. This can mean valuable time away from your job or school.
The most important point, however, is that skin problems are preventable. By eliminating the causes of skin sores and with routine inspection of your skin, skin sores need not happen. You must be responsible for your skin care. You must know the condition of your skin and the early warning signs of skin sores. Skin management cannot be neglected. Skin management is of vital importance to you and your continued ability to function.
Causes
Because your blood flows more slowly after SCI, your healing ability is reduced. In addition, your skin cannot tolerate as much pressure as before. Your skin can now tolerate a minute amount of pressure for a long time, but it can only tolerate great pressure for a short time before the circulatory system is disrupted and a pressure or skin sore results.
The decrease in circulation and lower tolerance for pressure is further aggravated by the lack of sensation after SCI. This lack of sensation means there is no longer a feedback mechanism to tell you that there is a problem – that you have been sitting too long without moving or that you have injured yourself, for example.
The major causes of skin sores are:
- Prolonged pressure
- Bruises or scrapes
- Prolonged wetness on the skin
- Burns
- Sitting or lying on hard objects
- Frostbite
Prolonged Pressure
Prolonged pressure means you sit or lie in the same position long enough to cause symptoms of skin damage. These symptoms can also be caused by any clothing, braces, or hard objects that put pressure on your skin. The first symptom – your warning signal – is a reddened area of the skin. No damage has occurred if you remove the pressure and the redness fades with 15 minutes after the pressure is removed.
Skin damage from pressure usually begins over bony prominences – any place on the body where the bones are close to the skin surface, such as the hip. Bony prominences tend to put pressure on the skin from within. If there is a firm surface on the outside as well, the skin will be pinched between the firm inside bone and the firm outside surface, resulting in a lack of circulation.
Due to the decrease in the rate of circulation that occurs following SCI, there is also less oxygen to the skin. This contributes to a lowering of the skin’s resistance. If the skin is deprived of oxygen due to pressure, the body will try to compensate by sending more blood to the area. This may result in swelling, which will put even further pressure on the blood vessels and further block circulation.
You have seen the impression left on a carpet after a chair was moved, and you know that the carpet will get a hole in it if the chair is not moved every so often. This same process happens a lot faster in people than in carpets. Pressure forces blood out of the tiny blood vessels, which nourish the skin and the tissue under the skin. The pressure is most likely to cause damage over bony parts of your body.
Bruises or Scrapes
Bruises or scrapes can occur as a result of a bump or fall. Other causes are ramming your feet into doors or walls or dragging your buttocks while transferring. Because of the lack or decrease of sensation, you may not realize that an injury has occurred. Because of the changes in your circulatory system, you will not heal as quickly and a skin sore may develop.
Prolonged Wetness on the Skin
Possible sources of wetness are perspiration, stool or urine. Moisture of any kind can cause chafing, or excoriation, of the skin. Band-Aids may also cause an excessive accumulation of moisture under the protected area. Moisture prolongs the healing process. Prolonged wetness can lead to a loss of layers of skin which may result in a skin sore.
Burns
Burns can occur from heat, friction, chemicals or tape. Possible sources of burns include:
- Sunburn
- Hot water, as in a bathtub or shower
- Hot water pipes
- Carrying hot foods or placing liquids on your lap
- Kitchen stove during the cooking process
- Picking up or touching hot foods or drinks, such as pizza or fried chicken
- Electrical appliances, such as hair dryers or irons
- Electric blankets, hot water bottles or heating pads
- Sunlamps
- Cigarettes
- Sitting on hot objects, such as rocks or concrete in the sun
- Hot pavement
- Automobile mufflers, tailpipe, exhaust, heater vents that are directed at the feet, seat-belts, steering wheel, upholstery, or any object that can get hot in a car
Friction burns can occur when surfaces rub against a hard surface, i.e. from spasm or sitting in bed at a 45-degree angle. Some chemicals, such as disinfectants, can cause burns, and adhesive tape can also cause burns (use the non-allergic type), “paper tape”.
Sitting or Lying on Hard Objects
Sitting or lying on a hard object can cause a skin sore. Possible sources are:
- Safety pins,
- Curlers or bobby pins
- Buttons on mattresses
- Buttons on jeans or slacks
- Bulky seams
- Objects placed in slacks’ pocket
- Catheter connectors
- Catheter clamps
- Tight pants over catheter tubing
Frostbite
Frostbite can occur as a result of exposure to a cold environment without enough protection. Always dress warmly if you are going to be outside in cold weather. Ice packs are also a source of frostbite if they are not used properly.
Other Things that Increase Your Chance of Getting a Pressure or Skin Sore:
- Skin wet from sweat, urine or stool
- Poor nutrition causing anemia (low blood count) and low protein
- Slouching in bed or in the wheelchair
- Fevers
- Bumps or other injuries to the skin
- Friction to the skin, caused by sliding or being pulled across a surface, or by spasms
- Clothing, braces, splints, etc., that are too tight
- Forgetting or neglecting to take care of yourself if feeling depressed or when drinking too much alcohol or abusing drugs
- Worn out or improper equipment
A skin sore begins as a red area on the skin. This reddened area may or may not feel hard and/or hot. If you have black skin, the area may appear shiny instead of red. At this stage, the progression is reversible. You must remove all pressure from this area until the skin returns to its normal color.
If pressure is not removed, a blister, pimple or scab may quickly form over the hard red area of the skin. This hard red area of skin means that the tissue underneath is dying. At this point, remove all pressure over the area and consult your physician.
In the next stage, a hole or ulcer forms in the dead tissue. Frequently, this dead tissue is small on the skin surface, but large in the deeper tissues. This damaged tissue may extend all the way to the bone.
And finally, there is infection and destruction of the underlying bone.
How a Pressure Sore Develops
Pressure sores are always caused by pressure.
| Stage & Signs | What to Do | Other Information |
|---|---|---|
| 1. Skin becomes white or lighter in color | Do push-ups and keep to your turning schedule so skin is never deprived of its blood supply for a long time |
|
| 2. Skin reddens, is warm and may be swollen when pressure is relieved |
|
|
| 3. A blister develops over red area. Skin may have a bluish color to it. The blister often opens |
|
|
| 4. Center of open sore turns black or brown and/or there is drainage |
|
|
Prevention of Skin Sores
You Can PREVENT Skin Sores. In order to prevent skin sores, you must:
- Check your whole body frequently
- Relieve skin pressure
- Take routine care of your skin
Check your whole body, but pay special attention to bony areas
By inspecting your skin regularly, you can spot a problem at the very beginning. Checking your skin is your responsibility and the way to spot the warning signals of a problem. Don’t just ask someone else how your skin looks. If you need someone to help you check, you must be able to tell him or her what to look for.
- How Often? — At least twice daily. Morning and evening when dressing or undressing are recommended. Check more frequently if you are increasing sitting or lying times. Checking whenever you change position is recommended.
- Watch For? — Any areas previously broken and healed over – scar tissue breaks easily.
- What Are You Looking For? — Redness, blisters, opening in skin, rashes, etc. Feel for heat in red areas with the back of your fingers.
- Equipment Needed? — Long-handled mirrors. If you need help, ask someone to position mirrors for you – one at the head and one over the pressure point.
Skin Check
- Which Parts To Check? — Check the following places on the front, back, and sides of your body. Remember: Bony areas of the body are the most likely to get sores, so be sure and look at them. When checking you skin, don’t forget your groin areas for rashes or sores from tight clothing. Men who wear an external catheter should check the penis carefully for sores or irritations.
Relieve Skin Pressure
In addition to routinely checking your skin, a second important way to prevent pressure sores is to relieve skin pressure by changing position or being positioned so that pressure is taken off a bony area. The purpose of relieving pressure is to let the blood supply get to the skin. If pressure is not relieved, blood will continue to be pressed out of a blood vessel and will not get to the skin to keep it healthy.
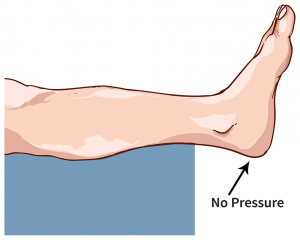
How to Relieve Skin Pressure from the Foot
Pillows can be used for offloading heel pressure in bed. It is recommended that pillows be placed length-wise under the calf to completely elevate the heel off the supporting surface.
Devices made of sheepskin, splints and bunny boots are all acceptable for offloading pressure. These devices pad the heel and prevent friction and shear.
How to Relieve Skin Pressure in Bed
Turning Schedule
Use a turning schedule that does not allow redness to appear on bony prominences. Depending on your body type, you will tolerate a turning schedule of two to five hours (turning from side to back to side). The length of time between turns can be gradually increased by adding 30 minutes to the amount of time in a given position and then checking for redness.
You will be asked to provide an alarm clock or some other means of awakening yourself for position changes during the nighttime. Ultimately, it will be your responsibility to either independently position yourself or verbally direct your caregiver to perform the task.
The only exception to a turning schedule is lying prone (on your abdomen).
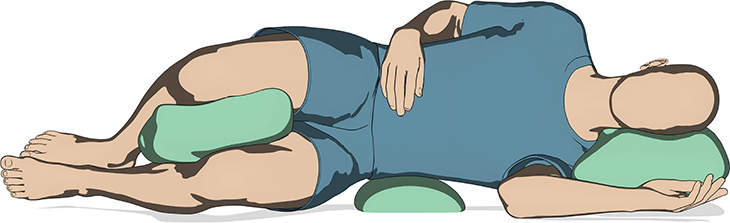
Prone Position Padding
You can safely lie prone for up to eight hours by using plump, firm pillows and small foam pads.
- Head — Small, foam support under head. Size of foam depends on individual comfort. Cover support with materials that are not irritating to your skin.
- Chest — Use one or more pillows according to comfort.
- Thighs — Foam pads placed above the knees to prevent redness of knees.
- Shins — Pad(s) or Pillow(s) under shins to elevate feet height enough to avoid pressure on toes (helps prevent ingrown toenails). An alternative is to allow toes to hang off the end of the bed. Feet should be at right angle to the legs per illustration above.
- Between Knees — Pads placed between knees to keep knees and ankles apart so pressure sores do not develop.
Warning: Do not substitute folded towels or blankets for foam padding or pillows. These can be too firm and cause skin breakdown.
Sleeping prone at night is very important for two reasons:
- Both you and whoever helps you to change your position can have a restful eight hours sleep without interruptions.
- Lying prone straightens your hips and helps prevent tightness of the hips and knees.
Alternate positions are side-to-side positioning as well as supine (back) position. Which position works to your benefit will be determined individually.
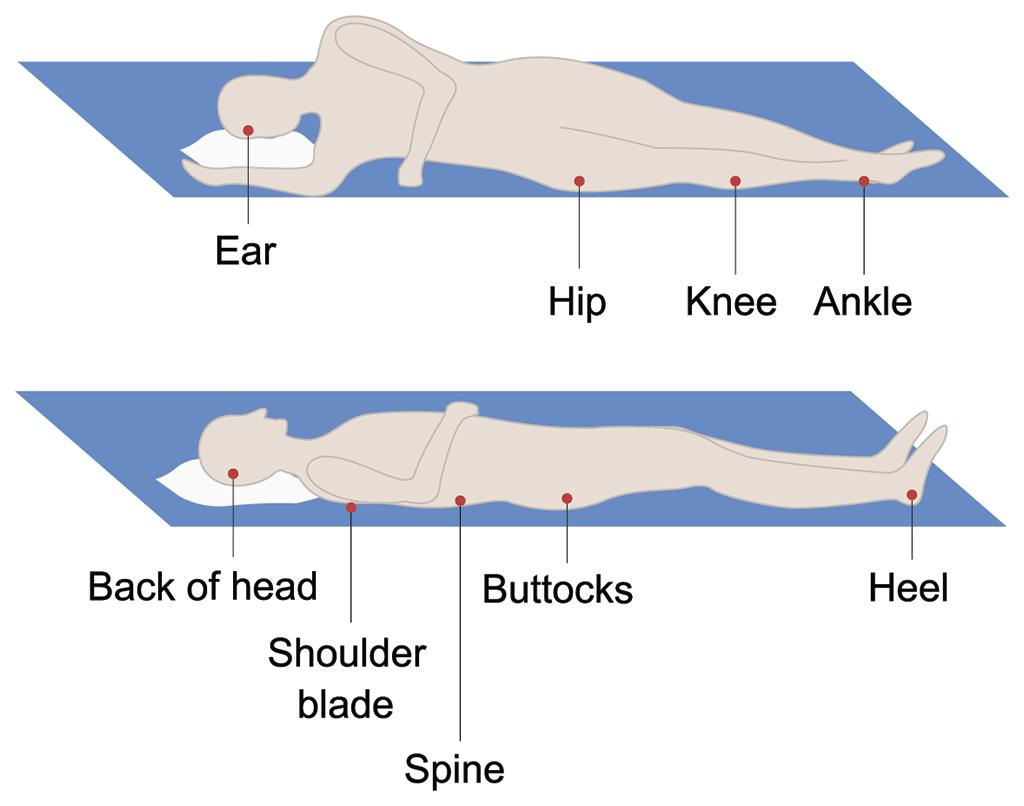
Side Position Padding
Position Padding with pillow behind the back.
- Head — Small, foam support under head. Size of foam depends on individual comfort. Cover support with materials that are not irritating to your skin.
- Back — Support behind back to maintain side position. Be sure bottom hip is pulled back to prevent rolling backwards on sacrum.
- Hips — Pad placed above and below the hip joint. When pads are placed correctly, a flat hand can be slid between the body and the bed to be certain that pressure has been relieved. If the pressure has not been relieved, an additional pad can be added.
- Ankle — Pad placed above the ankle joint.
- Between Lower Legs — Pillow placed lengthwise between legs to prevent pressure on the knees and ankle joint. Do not have legs directly on top of each other.
Warning: Do not substitute folded towels or blankets for foam padding or pillows. These can be too firm and can cause skin breakdown.
Supine (Back) Position Padding
- Head — Small, foam support under the head. Size of foam depends on individual comfort. Cover support with materials that are not irritating to your skin.
- Back — Place pad under lower back to provide elevation of the sacrum (tailbone). This will relieve pressure on the sacral area and relieve muscle tiredness in the back.
- Knees — The bend at the knee is a natural curvature. Use a pad above the area behind the knee. The pad must not be in the area behind the knee.
- Ankles — A small pad is necessary at the back of the heel to relieve tension on the calf of the leg. Also, the heels must be off the bed to prevent skin breakdown.
- Feet — A soft foot support is placed to allow simulation of weight bearing on the ball of the foot.
- Between Lower Legs — Foam pad or pillow placed between the knees to present possible breakdown at the knee and ankle joints.
Warning: Do not substitute folded towels or blankets for foam padding or pillows. These can be too firm and can cause skin breakdown.
How to Relieve Skin Pressure in a Wheelchair
Weight Shifts:
Weight shifts are the most essential techniques for preventing pressure on the skin and muscle of the sacrum (tailbone) and each hip. Use the method you and your therapists have found to be the most effective for you. Know your skin tolerance at all times. The frequency with which you do weight shifts vary from time to time.
Cushions:
A cushion for your wheelchair is essential. Cushions provide pressure relief and weight distribution and thus aid in the prevention of pressure sores. Many types of cushions exist, but there is no “ideal” cushion. Use the cushion recommended by your physical therapist/physiatrist.
- If air is used in the cushion, check to see that it is filled correctly. If you are going to a different altitude, there will be a change in your cushion.
- If your cushion is made of foam, check to see that it is firm and in good condition. If it gets dry, powdery and loses its firmness, replace it immediately. Use only good quality foam. Polyurethane foam with a density of 1.2 and compression of 30 to 35 is recommended.
- In case of body weight change, you may need to change the width of your chair, the frequency of your weight shifts, and the type of cushion you use.
Never use rubber air rings or rubber doughnuts. They are dangerous because they block the flow of blood to the skin inside the leg.
Weight shifts are essential. The cushion alone will not prevent pressure sores.
In Addition:
- Make sure the foot pedals of your wheelchair are adjusted to the right height for you. If your foot pedals are too high, it will put pressure on your hips;
- Sit up straight in your chair. Slumping or slouching leads to added pressure over the end of your tailbone.
- Lean to One Side
Take Routine Care of Your Skin
The third way to prevent skin sores, the most serious problem in SCI, is to keep your skin healthy. Health skin is skin which is intact, well lubricated with natural oils, and nourished by a good blood supply. Skin stays healthy with good diet, good hygiene, regular skin inspection, and regular pressure relief. We’ve already discussed skin inspection and pressure relief. We’ll focus here on hygiene and nutrition.
Hygiene -You must keep your skin clean and dry. Skin which is frequently moist from urine, sweat, or stool is more likely to break down. Dry skin well after bathing, but don’t rub hard with a towel as rubbing can damage the skin. You may have heard that alcohol massages over bony areas are good for you. They are not. Alcohol dries out your skin and dried, cracked skin is not healthy. If back rubs help you to relax, a gentle one with lotion should be given.
Diet and Fluids – Adequate fluids and a well-rounded diet provide nourishment to the skin. With a good diet containing protein, iron, and vitamins, your skin gets what it needs to stay healthy.
More Tips to Prevent Skin Sores:
Do:
- Make sure your wheelchair foot pedals are adjusted to the right height
- Use a prescribed cushion on wheelchair seat
- Sit up straight in wheelchair (slumping or slouching leads quickly to early skin breakdown over tailbone)
- Check feet carefully when wearing new shoes – shoes should not be too tight or too large
- Apply support hose and Ace wrap evenly so that they don’t wrinkle and cause extra pressure
- Keep skin clean and dry – urine allowed to stay on the skin can lead to problems
- Use a firm (not hard) mattress, which provides support for your body. Foam mattress over regular mattress helps to spread weight a little more evenly.
- Lie prone to keep hips stretched out. Also, this position spreads pressure more evenly and there is less chance to get sores
- Do your wheelchair push-ups or weight shifts every 15 minutes
- Stick to your turning schedule
- Use lubricating cream if you have dry skin
- Remember: even tiny shifts of position help somewhat
Do Not:
- Use a rubber air ring or any kind of doughnut – they create a lot of pressure where you don’t want it, and block the flow of blood to skin inside the ring.
- Wear sanitary belts – they can lead to pressure sores.
- Wear clothing with heavy seams, nylon underwear or tight clothing.
- Put articles in pants pockets or on seat of wheelchair.
- Use alcohol on dry skin.
- Sit in bed with the head raised for long periods – this causes skin to be squeezed over the lower end of the spine and can lead to sores

Majority of this content is from: PoinTIS